There is considerable global interest in the use of biological methods to regenerate damaged joint surfaces, and knee surgeons are gaining perspective as to how they can practically introduce such methods into their own practice.
What they are wanting is something that is preferably a 'one-step' technique, effective but simple, not exorbitantly expensive for their patients, and which helps to reduce knee pain and improve function in that group of patients who are younger and not on the list for a knee replacement.
Microfracture
Microfracture looked like it would be the answer. The technique was pioneered by Dr Steadman a decade and a half ago. Damaged cartilage cannot readily heal itself, because new cartilage cells have to come into the tissue from the deeper layers and when these are destroyed there is no way that the cartilage can heal itself. Dr Steadman showed that by poking an awl through the bony layer underneath the cartilage blood (and stem cells) could move up through the hole and cover the cartilage defect. In fact this technique was a sequel to a much earlier technique by Dr Pridie in the '50s, where he used small drill holes to achieve the same effect.
However, microfracture has not proved to be the miracle that it was hoped to be - there have been problems with the method. Firstly, patients had to be non-weight-bearing for several weeks to allow the new tissue to form, and if they became weight bearing too early all the benefit could be lost. Secondly, the tissue that did form was not as strong as the original cartilage. And then of course the inevitable happened, and the method became over-used and inadequately performed and sometimes caused even more damage that the original situation. Then an influential paper was published to show that prior microfracture actually prejudiced the outcomes of the more sophisticated cartilage plug procedures, such as ACI, and microfracture started to fall into some disrepute.
Recently, smaller awls and better spacing has led to the modified technique of 'nano-fracture'.
Stem Cell Procedures
The idea of using stem cells for cartilage repair, however, remained of significant interest to knee surgeons.
Stem cell procedures initially involved harvesting pluripotent (able to evolve into different cell types) cells from perhaps the bone marrow, multiply these up in culture in the laboratory, and then inject them into the knee. This was a 'two-step' procedure and very expensive.
A modification was to take blood from the patient during the surgical procedure, and pass it through a machine to separate off the fraction containing stem cells, and then to inject them into the knee. However, this required the machine to be available, and there were regulatory restrictions in some countries.
Adjuvant growth-stimulating factors, eg PRP
In addition to the procedures above, many clinics were adding to the cell preparation a blood fraction derived from the blood plasma - platelet rich plasma - which is very easily obtained from the patient's blood which is simply spun in a centrifuge. PRP has many chemical substances in it that stimulate cell division and tissue repair.
Pericytes and MSCs
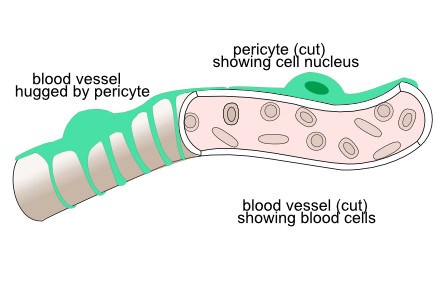
Relatively recent work has, however, revealed another interesting component to the story. The blood capillaries - the tiny vessels that supply oxygen to all the tissues - have little cells that hug onto the outer layer of the capillary - these are called 'pericytes'. These are little chemical factories that modulate immunology on the side nearest the vessel, and on the outer side they have release healing chemicals - anti-scarring, angiogenic (stimulate new blood vessels), mitotic (stimulate cell division) and anti-apoptotic (suppress cell death). Near the pericytes lurk quiescent stem cells.
The nerves that supply blood vessels - the sympathetic nerves - have been seen to actually be supplying the pericytes and not the actual cells of the blood vessel itsel.
Where there is blood vessel injury, the pericytes migrate off the blood vessel and become what are then called 'MSC's. The scientist who described these cells now wants these MSCs to be called 'Medical Signalling Cells' because they signal to the environment to heal the wound, releasing chemicals called cytokines and activating the quiescent stem cells to multiply and differentiate to restore the original environment.
One-step technique employing MSCs derived from body fat
A plastic surgeon has popularised a technique where - under sterile surgical conditions in the same operation - fat is sucked out from the abdomen area or inner thigh washed in saline, filtered, shaken in a syringe containing some little balls, filtered again (microfragmented fat), and then injected into tissues to encourage healing. The procedure encourages the release of the pericytes from capillaries in the fat, and the final filtrate is rich in MSCs and growth factors. The cells and chemicals are the patient's own - what we call autologous - so there is no rejection.
The most challenging part of the procedure is actually the taking of the fat sample. The procedure is similar to liposuction, and of course most plastic surgeons are confident with that technique, but it is unfamiliar to knee surgeons. So some surgeons are asking plastic surgeons to attend and perform that part of the procedure, while others perfer just to use the upper thigh where little harm can be done.
Dr Arnold Kaplan discussing his work and the work of Dr Carlo Tremolada on microfragmented fat, MSCs and pericytes.
