Children’s bones face the same propensity for injury and fracture as adults though the bones of children have are viewed in a very different manner as they are still dynamic with growth until sometime between 15-18 years of age when the physis or “growth plate” fuses and their injury approaches that of their adult counterparts.
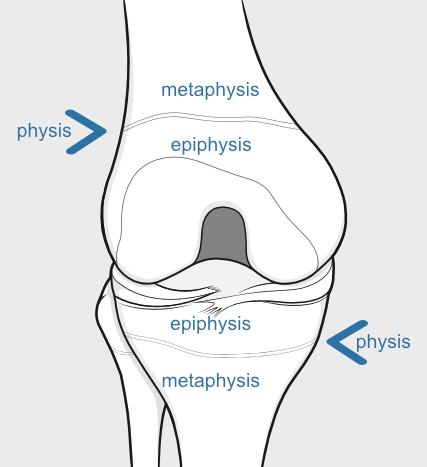
To get an understanding of the anatomy, let us take the femur or “thighbone” as an example. The femur has a proximal end, in the hip and a distal end in the knee. The bone has 2 growth plates which will appear on radiographs as non-ossified tissue, further hindering exam in many cases. The proximal growth plate of the femur has 2 “sides” the side of the shaft or the “metaphysis” and the side on the terminal side of the bone the “epiphysis”, these terms are very important in identification and implications for treatment. This may be thought of a “sandwich” with the cartilage growth plate in the middle, which is under the dynamic hormonal influence to growth during childhood and adolescence. A classification system termed the Salter–Harris classification exists to determine uniform criteria, identify the fracture (from I to V).
With children’s presence in team sports as well as the prevalence of general trauma children, they are at risk of a growth plate injury or fracture that involves the growth plate. Some 10-30% of fractures in children and adolescents involve the growth plate and it is important that it always be thought of and excluded or managed as if there is an injury that is not readily apparent in children with pain with movement of an extremity. Boys are twice as likely to sustain a fracture of this type. Growth plate injury usually comes from falls, trauma involved in playing team sports such as football. Injury to the growth plate can occur due to overuse injury as well in the case of say distance runners or gymnasts. Sadly injury can occur due to child abuse and motor vehicle accidents, less likely infection of the bone.
Assessing fractures in children (in addition to many other diagnoses) is difficult at times due to a lack of history. Often times, trauma is not witnessed, and younger preverbal or newly verbal children cannot give an adequate history. A high index of suspicion is essential in children who are unwilling to bear weight on a limb or allow an extremity to be moved or manipulated. A child or adolescent should not be advised to “work through the pain”.