Dr Smallman discusses the discovery that many cases of anterior knee pain are relieved by releasing the tethers restraining the fat pad and the infrapatellar plica.
 First published 2018, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
First published 2018, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
An alternative viewpoint on anterior knee pain - course
- CLINICAL CASES - Case 4
- CLINICAL CASES - Case 5
- BACKGROUND ANATOMY - Anterior compartment of the knee
- BACKGROUND ANATOMY - The Fat Pad
- BACKGROUND ANATOMY - The Infrapatellar Plica
- BACKGROUND ANATOMY - how the fat pad and infrapatellar plica form
- BACKGROUND PHYSIOLOGY - Kinematics of the knee
- BACKGROUND PHYSIOLOGY - Knee pain in general
- TAKEHOME MESSAGE - The surgical technique of Untethering the Fat Pad
A tenet of nature is that 'structure and function are linked'. In our research we set out to establish the link we had found between Anterior Knee Pain and untethering the fat pad
I. Structure
Anatomic dissection and histology
We examined structure by the anatomic dissection of cadaver knees, noting relationships. Basically, we disassembled 12 knees to see how the structures in the front of the knee work. I worked with Scott Ekroth at Upstate Medical University, to process specimens of the fat pad, and infrapatellar plica, from the Anatomic Donor Program. Dr. Kris Shekitka, a pathologist from the former Armed Forces Institute of Pathology, analyzed the microscopic slides from these specimens that allowed us to understand their roles at a cellular level. Key elements of this work are outlined in this course in the sections on BACKGROUND ANATOMY and in our presentation to the American Anatomy Association (ref. 1).
It seemed from our analysis that the enthesis organ concept could be applied to the knee, specifically to the contents of the anterior compartment of the knee, the fat pad and infrapatellar plica (IPP). The concept was conceived and published by a team of researchers, led by Michael Benjamin from Cardiff, Wales (ref. 2).
II. Function
Direct observation
Function can be implied through observation of mechanical behavior. We were able directly to observe the motion, and changing tension of the IPP and portions of the central body and fat pad through the arthroscope, and our observations suggested that these structures had a mechanical function (Video 1).
Indirect observation - volunteer studies
To visualize indirectly the behavior of the entire fat pad, central body and IPP, we used the radiographic tool of fluoroscopy and performed injection studies, approved by Upstate Medical University Institutional Research Board and reported online at: In Vivo Arthroscopic Behavior of the Infrapatellar Plica of the Knee. [Internet].; 2014, November 24. Available from: https://clinicaltrials.gov/ct2/show/NCT00643487 (link is external).
Volunteers, undergoing arthroscopy, were sedated, but could respond to command. Local anesthetic was used for the portals to insert instruments and the scope. Radiographic contrast material was placed into the central body and the outline of the IPP and fat pad (not an easy task), which, when filled, could be visualized using lateral fluoroscopy, allowing the creation of videos that demonstrate kinematic behavior (Videos 2 and 3).
Four screenshots from the video are shown in Figure 7 below:
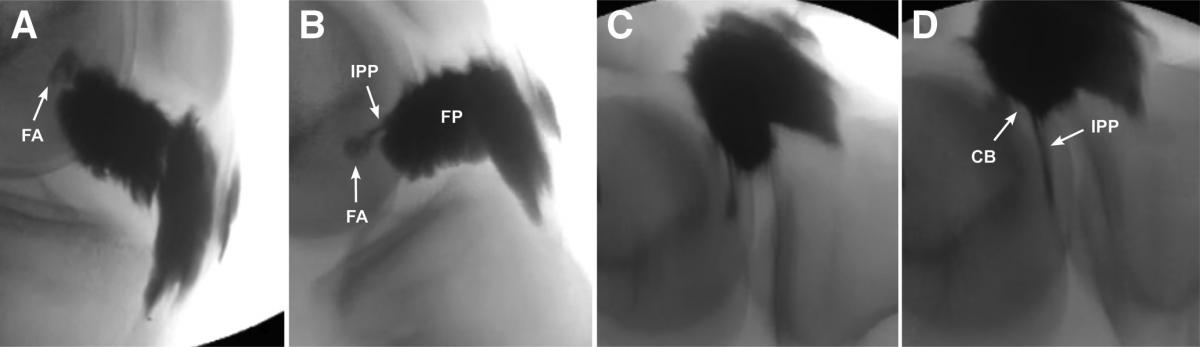
You can see that the fat pad (FP) distorts as the knee moves, tethered by the infrapatellar plica (IPP). The central body (CB) and IPP show remarkable stretch during terminal knee extension and completion of the “ screw home mechanism ":
- (A) 90° flexion: At the femoral attachment (FA) the IPP has a broad base, narrows and then disappears, hidden in the overlap of contrast of the medial and lateral extensions of the overlying fat pad; the overall shape of the fat pad is tubular, and elongated.
- (B) 45° flexion: The IPP is lax as attested by the ripple in its mid-portion; more of the IPP is visible. The fat pad shape has become compact.
- (C) Full extension: the IPP is stretched; the former broad base is less visible; the contrast has been squeezed out of the origin; The fat pad is now completely altered in shape.
- (D) Full extension plus “quads set” exercise: maximal effort at quads contraction by the patient produces even more stretch of the IPP, allowing visualization of the central body and further distortion of the fat pad.
Video 2 showed complete filling of IPP, central body, and IPP and Video 3 shows filling of IPP, central body, but just a portion of the fat pad. This eliminates the overlap of the medial and lateral extensions on either side of the central body, allowing the full stretch and deformity of the central body and IPP to be seen. Note that in video 3 the knee is facing the other way.
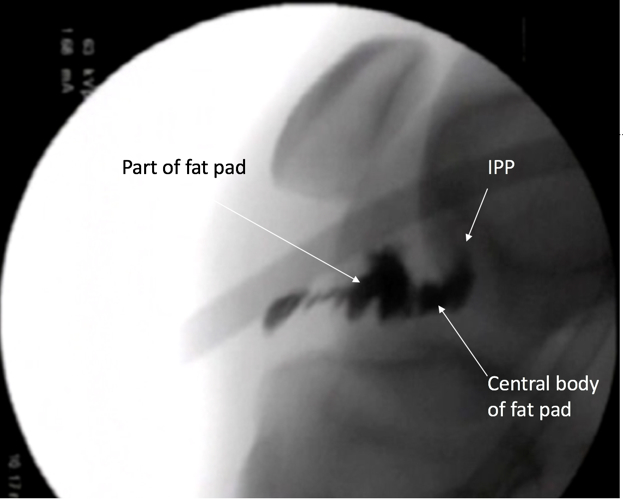
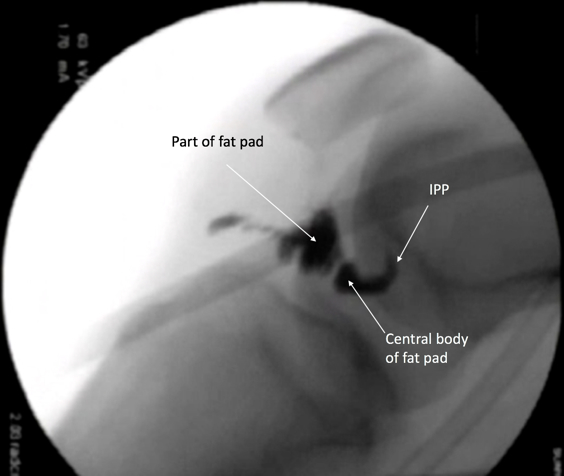
Three screenshots from the video are shown in Figure 8 below. Less contrast has been placed: only a portion the fat pad is seen. The central body and most of the IPP have filled. The broad base of the IPP has not filled and is not seen.
 |
 |
 |
| Figure 8A. The IPP is worm-like, much larger than in the previous case. It is vertical at 90°. The central body is now well seen, and not obscured by the overlap of the medial and lateral extensions. | Figure 8B. The IPP and central body have rotated and appear relaxed. There is slight change of the contrast within the fat pad, representing some distortion. | Figure 8C. The contrast has been squeezed out of the base region of the IPP. Both it and the central body are stretched and distorted. The contrast within fat pad has shifted. |
SUMMARY: The details in flexion are not well seen. The complex appears relaxed in mid arc, and then in terminal extension remarkable stretch and deformity of the IPP, central body is seen, along with a shift in the contrast within the fat pad.
The question then arising from these kinematic studies was: How does this unit become a pain generator?
The first key point has to do with physical location.
For joints to maintain stability, their supporting ligaments must maintain their fixed lengths as the joint moves around a small arc termed the instant center of rotation . The term for this characteristic of ligaments is that they are isometric. The stabilizing ligaments of the knee (eg the anterior cruciate ligament) maintain fixed lengths as they rotate around the instant center of rotation (ICR) of the knee, and they are thus isometric ligaments.
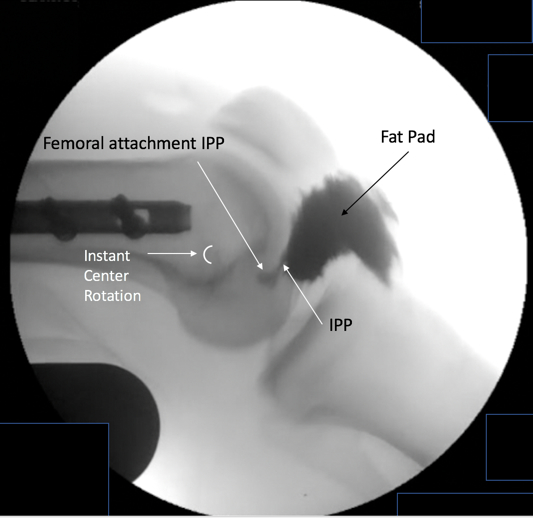 |
Figure 9. Our injection studies show the true kinematics of the IPP-fat pad complex, particularly the remarkable stretch and deformity in terminal extension proving that the IPP is non-isometric. The IPP must go through a cycle, stretching as the knee flexes, relaxing in mid-arc, and then stretching remarkably in extension, and even more if the knee is one that hyperextends. The IPP does not work in isolation. It is attached to the fat pad at the central body.The entire IPP-fat pad complex is thus non-isometric, leading to the stretch and deformity that the kinematic videos show. |
The second key point is the link between movement, applied force, stretch and deformation, and perturbation of noxious nerves contained within the fat pad.
This pattern of non-isometric mechanical behavior stretch and distortion of the ligamentous IPP and fat pad is confirmed in the kinematic videos and in Figures 5 and 6 which consists of screen shots from the fluoroscopies of volunteers in the In-Vivo study. Because the fat pad is tethered centrally by the IPP and to its wide fibrous attachment on its periphery, it is held captive within the borders of the anterior compartment.

Our studies, and those of others demonstrate that the fat pad is highly innervated, its nerves either protected in lobular fat or coursing within the elastic septa. The central body transition zone contains a network of neurovascular bundles lodged and also protected in the lobular fat between finger-like dense connective tissue bands that merge to become the rope-like central zone of the IPP. There are also sparse nerves in the plica itself. An orthopaedic surgeon, Scott Dye, heroically demonstrated the synovial membrane, lining the entire joint, is moderately to severely painful to physical pressure, and that the most sensitive tissues of all are the fat pad and immediately adjacent structures (ref. 3).
The basic structure of the fat pad is thus a fibrous scaffold (ref. 4), packed with lobules of compressible fat, highly innervated throughout. On its periphery anteriorly the fat pad is then widely and firmly attached to the fibrous capsule and patellar tendon. It is tethered centrally by the IPP which is, as we have confirmed, a non-isometric ligament (ref. 1). The anterior compartment borders are bony and cartilagenous on 3 sides and firm fibrous capsule and ligament in front. As the knee moves, the geometrically complex borders constantly change. Tethered by the IPP between, the fat pad must stretch, relax and deform with knee motion. If the contained noxious nerves have been activated to a painful state by some pathology in the knee, the patient will perceive added pain related to this physical perturbation of these nerves.
Forces applied to and through the anterior compartment are seamlessly transmitted with appropriate attenuation through the IPP-fat pad complex to the apex of the notch via the central body and IPP, and to the tibia via the inferior dense connective tissue (DCT) bands.
We were able to demonstrate effect of these connections in vivo in the volunteer study by asking the patients to do a “quads set” manouevre, maximally contracting the quads with the knee locked in full extension. The patella moves about a centimeter as the 18-year-old volunteer “gets it” contracting forcefully her quadriceps in knee-locked position.
Untethering of the fat pad
Once untethered by release and resection of the IPP the kinematic videos confirm that the untethered fat pad shows virtually no stretch and distortion. This correlates with absolute pain relief. With motion eliminated in the quads set, it is the connective tissue links in the synovial layer, the alar folds, and the superior dense connective tissue bands that transmit these forces.
In Figure 9 below, the fat pad fills the anterior compartment, its contour matching the curves of the condyles and occupying the notch, as well, in full flexion. Virtually all of the deformation and stretch of the IPP-fat pad complex has been eliminated. The radiograph represents gross anatomy. These videos thus provide radiographic correlation between the clinical problem of AKP and the structure of the IPP-fat pad complex. Untethering the fat pad allows it simply to fill the anterior compartment without painful eccentric distortion and stretch.

Figure 10. Kinematics of the IPP-FP complex after release of the IPP; screenshots from Video 2. The cyclical stretch, and relaxation of the IPP, plus the distortion and stretch of the central body and fat pad has been abolished by release of the IPP at the femoral attachment. The fat pad fills the available space without the distortion visible when the IPP is present. The IPP and femoral attachment are simply not seen post release and partial resection.
References
1. Smallman T, Shekitka K, Mann K, Race A. The Infrapatellar Plica - a New Non-Isometric Intra-Articular Ligament of the Knee. The FASEB Journal. Volume 29, Issue 1, supplement Apr 2015: 865.16
2. Benjamin M, Moriggl B, Brenner E, Emery P, McGonagle D, Redman S. The “enthesis organ” concept: why enthesopathies may not present as focal insertional disorders. Arthritis Rheum. 2004;50(10):3306-3313.
3. Dye SF, Vaupel GL, Dye CC. Conscious neurosensory mapping of the internal structures of the human knee without intraarticular anesthesia. Am J Sports Med. 1998;26(6):773-777.
4. Swan A, Mercer S. Anatomy of the infrapatellar fat pad. New Zealand Journal of Physiotherapy 33(1) 19-22. 2005;33(1):19-22.
5. Bohnsack M, Meier F, Walter GF, Hurschler C, Schmolke S, Wirth CJ, et al. Distribution of substance-P nerves inside the infrapatellar fat pad and the adjacent synovial tissue: a neurohistological approach to anterior knee pain syndrome. Arch Orthop Trauma Surg. 2005 Nov Nov;125(9):592-7.
PREVIOUS PART: BACKGROUND ANATOMY - how the fat pad and infrapatellar plica form
NEXT PART: BACKGROUND PHYSIOLOGY - Knee pain in general
