Dr Noyes discusses the options in 'salvage' cases after knee arthrofibrosis.
 First published by Dr Noyes in 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
First published by Dr Noyes in 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
A salvage is a colloquialism.
A salvage means that the surgeon can not reliably predict by scientific data what the benefits will be to the patient and that means that it is getting to the last resort and the patient may be benefited or may not achieve a benefit.
Open z-plasty, medial-lateral retinacular tissues
The principal of a z-plasty technique is to preserve the function of the medial and lateral retinacular soft tissues and, as well, debride the tissues to a normal thickness.
The operation includes a thorough removal of contracted tissues around the patella, while protecting the patellar tendon, and a lengthening technique of contracted medial and lateral patellar tissues.

The figure shows:
A, Preoperative examination under anesthesia of a patient with established arthrofibrosis shows a complete lack of patellar mobility, absent medial and lateral glide, and an obvious patella infera with shortening of the patellar tendon. The range of motion was 0/0/80°.
B, The medial retinaculum and soft tissues were split in a z-plasty fashion to allow a loose closure and restore a normal medial patellar glide. An arthroscopic procedure was performed just before the open procedure to re-establish the suprapatellar pouch, remove intra-articular adhesions within the suprapatellar pouch and medial and lateral tibiofemoral gutters, and document the condition of the joint.
C, Completion of medial z-plasty release shows the medial soft tissue flaps that were developed. A debridement of infrapatellar scar tissue was performed under direct visualization.
D, A lateral z-plasty release of contracted lateral retinacular tissues was performed.
E, The loose closure of the lateral z-plasty release allowed restoration of a normal medial patellar glide.
[Noyes FR, Barber-Westin SD: Chapter 41: Prevention and treatment of knee arthrofibrosis. This article was published in Noyes’ Knee Disorders: Surgery, Rehabilitation, Clinical Outcomes, Noyes FR, Barber-Westin SD (eds.), pp. 1053-1095, Copyright Saunders, 2009.]
Posterior Medial-Lateral Capsulotomy
I would say that I see some of the worst knees that have been out 3-4 months to a year, that are at 15 degrees and a hard end point, or even 20-25 degrees - and these knees absolutely require posterior releases to protect the joint.
I was on the KNEEguru website, and I have been on others, and you will see the question commonly come up “I came in at 10-15 degrees, my surgeon got me to almost 5 degrees and then it entirely came back”. The reason it is coming back is that those posterior capsular tissues are very very thick and you will stretch them out, but only part way - and that is probably the number one reason for recurrence or why the therapist is not able to get 0 degrees (after you have made sure that you have cleaned out the notch and you have no scar tissue in the notch).
Open posterior capsulotomy (cutting open the capsule behind the knee) may be an option to allow full extension of the knee joint (there may be soft tissue calcification in the capsule and posterior structures). This procedure then requires outpatient serial extension casting - replastering the leg to force full extension.
The posterior capsule releases are also accompanied with an arthroscopic procedure to remove any tissue that has grown into the notch that would also block extension.
The Figure shows a patient with arthrofibrosis (0-15-80°) requiring an arthroscopic lysis of adhesions, parapatellar releases, and posterior medial and lateral capsulotomy for the 15° flexion contracture.

[Noyes FR, Barber-Westin SD: Chapter 41: Prevention and treatment of knee arthrofibrosis. This article was published in Noyes’ Knee Disorders: Surgery, Rehabilitation, Clinical Outcomes, Noyes FR, Barber-Westin SD (eds.), pp. 1053-1095, Copyright Saunders, 2009.]
A, An arthroscopic lysis of adhesions, removal of scar tissue, and parapatellar releases was performed first. All scar tissue from the notch region was removed and a notchplasty done so that these tissues did not block extension.
B, The medial joint line was marked.
C, A posteromedial incision was made.
D, The approach reflecting the sartorius was used as we have described for an inside-out medial meniscus repair.
E, A vertical posteromedial capsulotomy was made directly behind the superficial medial collateral ligament.
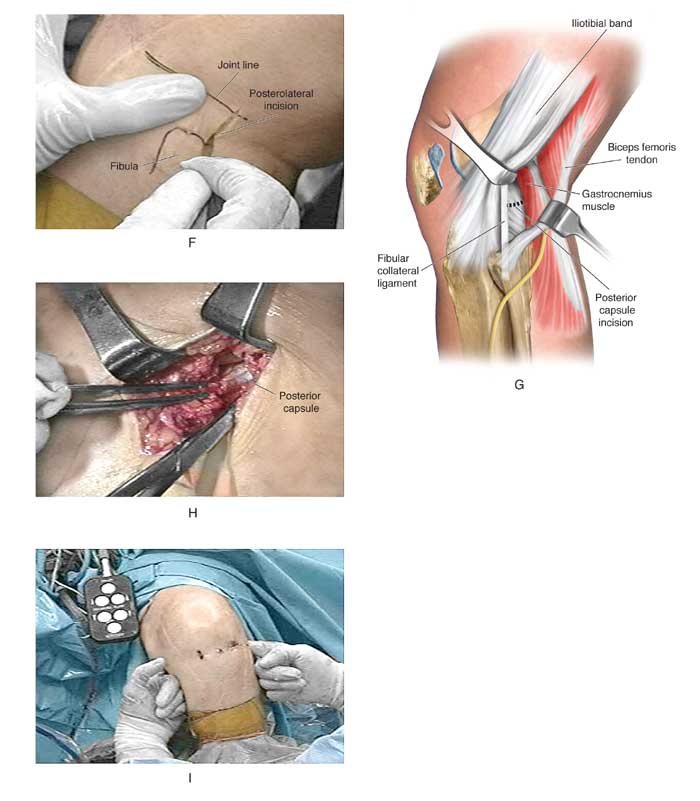
F, The posterolateral approach for a capsular release used the same approach as a lateral meniscus repair with a skin incision just distal to the joint line as shown.
G, The posterolateral capsule anterior to the gastrocnemius tendon was identified.
H, The posterolateral capsule was carefully incised under direct visualization to the edge of the lateral femoral condyle, avoiding the neurovascular structures.
I, A finger was placed into the posteromedial and posterolateral incisions and the central neurovascular structures were palpated. The central posterior capsule anterior to the neurovascular structures was not released. The finger palpation confirmed that the capsule directly posterior to the medial and lateral femoral condyles had been incised, removing this block to extension as the knee was extended.
The remaining posterior capsular tissues were then gently stretched with the overpressure program described in another part of this course to achieve extension.
PREVIOUS PART: Arthroscopic surgery (for arthrofibrosis)
NEXT PART: Rehabilitation After Operative Procedures for Arthrofibrosis
