The different cartilage repair procedures can be a bit confusing to patients, but Dr Hambly explains thae rationale behind them.
 First published in 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
First published in 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
Which articular cartilage repair procedure?
There are a number of articular cartilage repair procedures in general use at present and a lot more in development.
The selection of a procedure can be quite confusing especially if you are given several options by your surgeon. One of the reasons for this is that selecting an articular cartilage procedure isn't black and white and the different procedures often overlap with each so that there may be more than one option available to you.
Articular cartilage repair procedures may differ in the technologies and surgical techniques that they use but they all share a common philosophy of repairing articular cartilage whilst keeping options available in case you need them in the future. In this way you don't 'burn your bridges' by opting for an articular cartilage repair procedure.
There are some contraindications to articular cartilage repair procedures with the three main ones being advanced osteoarthritis, rheumatoid arthritis and total menisectomy. In addition, articular cartilage repair should only take place if any mechanical malalignment and ligament laxity is either corrected prior to or at the same time as the articular cartilage repair procedure.
For all articular cartilage repair procedures your surgeon will need to gain your informed consent to the procedure and you must be willing and able to commit to and complete the rehabilitation programme.
Articular cartilage repair procedures can be broadly categorised into four groups as follows:
Arthroscopic Lavage and Debridement
These are procedures that are carried out via 'keyhole' (arthroscopic) surgery. Lavage is basically washing out the knee joint and debridement is removing any unstable or degenerative articular cartilage flaps. These can be useful palliative treatments to reduce pain, mechanical irritation and inflammatory mediators but any benefits tend to be short-term only. Although these procedures are invariably classed as treatment options for articular cartilage damage they should not be viewed as articular cartilage repair procedures. They can't be articular cartilage repair procedures as they don't repair the articular cartilage - they give the knee joint a bit of a clean-up. The main group of patients that often receive some benefit from this procedure are those patients with very small defects (less than 1cm2) and localised mechanical symptoms due to small flaps or loose pieces of articular cartilage.
Marrow Stimulation Techniques
These surgical techniques have been around for almost half a century. All the techniques that fall under marrow stimulation are based on two key steps.
- The removal of damaged cartilage to expose the underlying bone.
- Penetration of the subchondral bone to expose the blood vessels and generate a blood clot within the defect.
The older marrow stimulation techniques used abrasion and/or drilling using fine wires to penetrate the subchondral bone. There are disadvantages with these techniques though as the heat produced by the abrasion/drilling can cause cells to die (necrosis). Twenty years or so ago the newer technique of microfracture was introduced where, instead of motorised, heat producing tools, a fine bone pick (awl) is used to punch into the subchondral bone at 2-3-mm intervals to a depth of 2-4mm.
Microfracture is frequently used as a first line treatment for articular cartilage defects in younger patients (<30-40 years) with a small (<2cm2) isolated chondral defect. The reason for this is that microfracture is generally an arthroscopic procedure and if the microfracture doesn't work it is possible to move onto another, but usually more invasive, cartilage repair technique.
Studies have shown that microfracture techniques often don't fill in the chondral defect fully and the repair material is fibrocartilage which is not as good mechanically as hyaline cartilage. The blood clot is very delicate after surgery and needs to be protected. In terms of time, the clot takes about 8 weeks to convert to fibrous tissue and is usually fibrocartilage by about 4 months post surgery. This all has implications for rehabilitation that will be discussed in a later section.
Defects as a result of a sudden injury seem to do better than defects from wear and tear damage. Patients can often do well for 1 or 2 years after microfracture but then symptoms often start to return as the fibrocartilage wears away. However, for some patients the repair tissue doesn't wear away so quickly and this is why the technique is often used as an intermediate step. If it works- fantastic, if it doesn't then you can move onto another articular cartilage repair procedure. However it is always worth bearing in mind that there is an increased risk of problems with multiple surgeries.
Osteochondral Autografts and Allografts
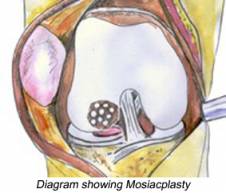
Sometimes you will see this type of procedure also referred to as 'OATS' (osteoarticular transfer system) or 'mosaicplasty'.
Osteochondral Autograft Transfer
Cylindrical plugs of articular cartilage attached to subchondral bone are taken from a non-weighting bearing area of the knee such as the edges of the femoral condyle with an instrument similar to a small apple corer. These plugs are then inserted into matching holes that have been drilled in the chondral defect. This is all completed during a single surgery arthroscopically where possible or if this isn't possible then via a small arthrotomy (open incision). The plugs are comprised of hyaline cartilage but the spaces around the plugs fill in with fibrocartilage as does the donor site.
One of the problems with this technique is something called donor site morbidity - that is what happens to the area that the healthy tissue plug was taken from after the surgery. In effect OATS is a bit like 'robbing peter to pay paul' and consequently it is often limited to chondral defects less than 4cm2 in size. The patella also presents an additional challenge due to the unique stress and loads that the patella has to accommodate.
Osteochondral Allografts
This is basically the same procedure as osteochondral autograft but instead of getting the plugs from your own body they are taken from a deceased donor. One of the advantages of using allografts over autografts is that more osteochondral tissue can be taken so larger areas of defects can be repaired. However, allografts are often not available or are very difficult to come by in some countries.
A recent progression to osteochondral allografts is the development of a procedure called 'Mega-OATS'.
Mega-OATS is version of osteochondral allograft where a single large plug is used to fill larger chondral defects. Mega-OATS is not widely used at present but where it is it is reserved for younger patients with large chondral defects.
For all of the variations of osteochondral grafting the surgical technique is important as with all articular cartilage repair procedures. The plugs should be flush with the surrounding articular cartilage and ideally should be positioned so that they follow the contours of the articular surface.
Autologous Chondrocyte Implantation
In the past articular cartilage repair procedures have tended to generate fibrocartilage repair tissue or, at best, a combination of hyaline and fibrocartilage repair tissue. In the 1980's the first orthopaedic tissue-engineered cartilage repair procedure was introduced - autologous chondrocyte implantation or ACI - with the aim of providing a hyaline repair tissue. Over the last 20 years the procedure has become more widespread and it is currently probably the most researched articular cartilage repair technique. At present most ACI procedures are in two stages:
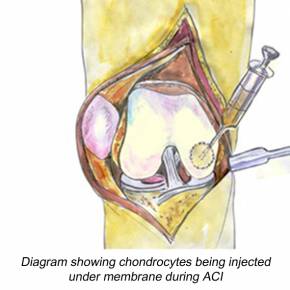
- Stage 1: The first stage involves an arthroscopic assessment of the chondral defect. If the defect is suitable for ACI then a small sample of cartilage is taken from a non-weight bearing area of the femur. This sample is sent to a specialist laboratory where the cartilage cells (chondrocytes) are nurtured and encouraged to multiply until there are a sufficient number to fill the defect (many millions). This usually takes between 3 and 6 weeks.
- Stage 2: The second stage is when the chondral defect is trimmed back to a point where all the surrounding edges are healthy cartilage and the underlying bone is exposed. Then the cells are reintroduced back into the defect. Unlike the first stage, in most countries at present, this stage is not arthroscopic - it is via an open arthrotomy.
ACI is an umbrella term for cell-based cartilage repair procedures and there are a number of variations with slightly different materials and/or surgical procedures. The first ACI procedure retained the cells in place using a cover of periosteum (a fibrous covering over the bone) from the tibia (shin bone) which is sutured (stitched) to the adjacent healthy cartilage to provide a watertight chamber into which the newly grown cartilage cells are injected. Periosteal ACI procedures have produced good results, sometimes too good, as the cartilage cells tend to overgrow in some patients and cause problems. In addition there is an extra incision needed to surgically remove the periosteum. Therefore scientists have developed membranes made of collagen that perform the same role as periosteum in order to reduce these problems. Variations of ACI that you may come across include CACI (collagen autologous chondrocyte implantation) where a collagen membrane is used to replace the periosteal tissue and the cells are injected into the chamber or MACI (matrix-induced autologous chondrocyte implantation) where the cartilage cells are seeded directly onto a membrane which is then glued into the defect. This is a fast moving area in medicine with new variations of the ACI technique emerging all the time.
There are a lot of differences in the ACI procedures that are available for patients across different countries. For instance in the USA at present the Food and Drugs Administration haven't approved the use of the artificial membranes that have been in use in Europe for several years now and some countries, Italy for example, are using arthroscopic techniques for ACI when most counties are still performing open surgery. In addition, ACI is expensive compared to other articular cartilage repair procedures due to the two stages and the cost of growing the cartilage cells and there are quite a few countries where it is difficult to get insurance companies to agree to ACI procedures.
Osteotomy
First of all osteotomy isn't an articular cartilage repair technique. So why is it in this section I hear you ask? Well because osteotomies are surgical procedures that can help to protect areas of articular cartilage damage and they are therefore commonly performed in conjunction with articular cartilage repair procedures. So what is an osteotomy?
Osteo is bone and otomy is to take away so an osteotomy is a procedure where the surgeon removes a wedge of bone from either your thigh bone (femur) or more commonly the shin bone (tibia). Osteotomies are techniques that are used to correct the mechanical alignment of the knee by surgically repositioning the joint. This is useful when you have articular cartilage damage in one area (compartment) as the osteotomy will help to shift some of the forces from the damaged part of the joint to the other side of the joint so giving some protection to the damaged side of the knee.
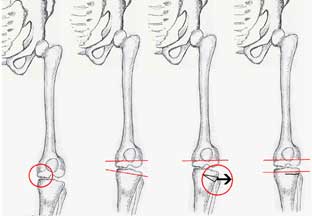
There are several different surgical techniques and you may come across the terms 'opening wedge' and 'closing wedge'. An opening wedge osteotomy means that a wedge is opened up where as a closing wedge osteotomy is where a wedge of of bone is taken out as shown in the diagram to the right. The choice of osteotomy will depend on what aspect of mechanical alignment needs to be corrected. The most common osteotomy that is used for patients with tibiofemoral malalignment is a high tibial osteotomy (HTO). For patients with patellofemoral (knee cap) malalignment the osteotomy procedure that is used is called either a tibial tuberosity osteotomy (TTO) or tibial tuberosity transfer (TTT).
It must be noted that an osteotomy isn't a solution to the problem of the articular cartilage damage but by off loading the damaged area it can help to delay its progression. If articular cartilage damage is present in both sides of the knee joint then an osteotomy isn't suitable. The rehabilitation is also lengthy. Therefore osteotomy is generally reserved for young, active patients.