Defining the various types of osteotomy relating to the knee.
 First published 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
First published 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
Part 2 - Osteotomy for varus and valgus deformity
- Indications for varus and valgus osteotomy
- Living with painful varus and valgus deformity
- High tibial osteotomy and distal femoral osteotomy
- Case study of high tibial osteotomy aiding ligament instability
- Benefits of varus/valgus osteotomy
- Potential problems with varus/valgus osteotomy
- Recovery post knee osteotomy
Part 3 - Osteotomy for patellar instability
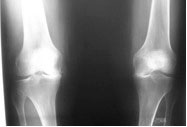
An osteotomy is a procedure where a bone is surgically cut - generally to allow the surgeon to realign the bone to a better anatomical position, in order to achieve improved function and/or alleviate pain.
Such an osteotomy is called a realignment osteotomy.
History
The procedure of osteotomy used to be somewhat less of an exact science than it is at present. It involved relatively unsophisticated instrumentation, as well as the use of fairly weak surgical fixation devices (plates and staples). These devices were used to fix the bone in the new, realigned, position, but they were not strong enough to allow the patients to mobilise normally following the surgery. The relatively weak fixation meant that patients had their legs placed into plaster casts following the surgery for at least 6 weeks. This meant that the knees stiffened up and the results of the surgery were less than optimal. In addition, the correction required to achieve realignment was often quite crudely calculated, sometimes by no more than eye-balling the lower leg during the operation.
Nowadays the surgery is very carefully planned, down to the last degree and the last millimetre, using specialist X-rays, specialist digital software and then using special instrumentation in the operating theatre to achieve very accurate results, which is then held totally rigidly with a revolutionary plate which was introduced by Alex Staubli 8 to 10 years ago. This plate permits immediate weight bearing and has eliminated the use of plaster casts.
Common osteotomies