This paper, by a distinguished group of specialists, effectively provides a European consensus on modern management of damage to the knee meniscus. The meniscus is an important structure, and damage may lead to faulty mechanics in the knee and ultimately post-traumatic osteoarthritis, and It was noted that the literature revealed "a rather low scientific quality of studies examining the treatment of traumatic meniscus tears", so an expert consensus like this is of great value in guiding practitioners in helping their meniscus patients.
This consensus only refers to 'traumatic' tears of the meniscus. The group defined a traumatic meniscal tear as one "with an acute onset of symptoms caused by a sufficient trauma" [injury], so that is what we are talking about here. This is to make a clear distinction between damage due to trauma as opposed to damage due to wear-and-tear degeneration.
A number of question-and-answer sets were prepared based on the medical literature, and then these were carefully critiqued to determine their scientific validity.
Key traumatic meniscus tears
The main types of meniscus tears affecting the function of the meniscus were identified as:
- vertical tears, such as longitudinal (including bucket handle)
- radial tears (including flap tears)
- posterolateral root tears
Meniscal ramp tears at the back of the joint were considered not to affect the actual meniscus tissue, so they were excluded from the evaluation. Horizontal tears were also excluded because the panel felt that they were primarily degenerative in nature from repetitive microtrauma and degeneration, even though they may be seen in younger patients.
Traumatic meniscal tears often occur in association with cruciate ligament tears.
Main surgical treatment options
The main surgical treatment options for traumatic meniscus tears were identified as:
- arthroscopic partial meniscectomy
- meniscus repair.
Several studies showed that meniscal repair leads to a higher level of activity and higher patient satisfaction in the long term. There are geographic differences in practice, but data from the USA shows that the percentage of meniscus repairs has increased by 37% per surgeon from 2004 to 2012, whereas the rate of meniscectomies has over the same time decreased by 17% per surgeon, but despite the improved numbers a significant mismatch has been identified between the incidence of repairable meniscus tears and the repair rates in clinical practice. Reasons may include the longer rehabilitation time for repair compared to meniscectomy, as well as the risk of repair failure and need for subsequent arthroscopy, although the clinical success rate of meniscus repairs substantially outweighs the failures, by 85%. The authors feel that there is still a lack of full understanding of the importance of repair over meniscectomy in the prevention of osteoarthritis.
What is the definition of a traumatic meniscus tear?
They defined a traumatic meniscal tear as one that is associated with a sufficient knee injury and a sudden onset of knee pain, which includes vertical and radial tears, flap tears and posterolateral root tears. Ramp tears did not altogether fit their definition and horizontal tears were considered to be primarily degenerative.
What is the definition of stable and unstable traumatic meniscus tears?
In an unstable tear the central part of the meniscus can become displaced or can be displaced with a probe. An unstable part may displace and cause joint locking and sudden pain.
What is the definition of a stable and unstable knee?
A stable knee has intact ligaments.
Which classification should be used to describe the location of a meniscus tear?
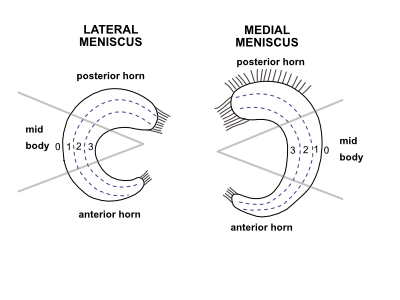
The panel felt that it is no longer appropriate to identify the position of a tear using vascular zones - eg red-red, red-white - and they advocate that the diagram below should be used instead to clarify exactly where the lesion is:
What is the incidence of traumatic meniscus tears in stable knees?
Meniscus tears were identified in 6.7% of acutely injured knees, with a higher incidence in men rather than women, and 75% of tears were in the medial meniscus.
What is the incidence of traumatic meniscus tears in unstable knees?
Acute ligament tears of ACL (anterior cruciate ligament) and ACL/MCL (medial collateral ligament) were more inclined to involve the lateral meniscus. Chronic tears of the ACL tended to involve the medial meniscus, and as many as 96% of patients with chronic ACL tears had sustained a meniscus tear!
What is the cause of pain in traumatic meniscus tears?
A meniscus tear generates pain from nerve receptors in the meniscus and the adjacent synovial tissue on the outer aspect of the meniscus, and pain-inducing chemicals are also released.
Are the clinical diagnostic tests accurate for assessing a meniscus tear of the knee?
The panel recommends that more than one test be used in clinical examination for meniscal tears. They recommend two tests in particular for their accuracy and specificity -
- McMurray joint line tenderness test
- Ege test [weight-bearing McMurray test]
- Thessaly test [reproduces joint loading in the knee]
Is an MRI systematically necessary in a knee with a suspected traumatic meniscus tear?
There was no consensus on this question, other than that a musculoskeletal specialist should be the one ordering the scan.. MRI may be a useful preoperative tool - if arthroscopy is to be performed anyway then it may help with pre-operative planning.
Has a consensus been established for the assessment of meniscus healing?
The panel notes that the most reliable technique to assess meniscus healing is arthroscopy.
Factors affecting the success rate of repaired traumatic meniscus tears
The panel considers that tears located in zone 1 have a statistically significantly better healing rate (87 to 91%) than tears located in zone 2 (59 to 79%), but still feel that that a tear in zone 3 should not be considered an absolute contra-indication for repair as sometimes a good result may be obtained.
Does the location of the traumatic meniscus tear (anterior or posterior horn or mid-body) play a role in successful repair?
The report notes that literature is scarce, but that the anterior-posterior position of tears does not seem to make a difference in outcome after surgery.
Does the length of a repaired longitudinal traumatic meniscus tear play a role in successful repair?
The panel considered the literature to be controversial, and that the surgeon therefore should not consider a long tear to be a contra-indication for repair.
Does the patient’s age affect the success of the meniscus repair?
The literature reports repairs from age 8 to age 58, and the panel found that age did not seem to affect outcome. However, they nonetheless caution that the surgeon should consider possible meniscal degeneration in the older patient.
Does the patient’s BMI or weight affect the success of meniscus repair?
The panel found that patients with a higher BMI (up to 35) do not appear to have a higher risk for failure of meniscus repairs.
Does the patient’s level of activity affect the success of meniscus repair?
The panel found this question proved still be controversial.
Does lower limb alignment affect the success of repaired traumatic meniscus tears?
There appears to be a lack of studies on this question, and currently a traumatic tear in a varus or valgus knee seems not to be managed any differently from that in a normal knee.
What is the fate of traumatic meniscus tears left in situ?
Studies here also appear to be few, but after reviewing the available literature the panel suggests that small tears (≤ 10 mm) of the lateral meniscus can be left alone and do not require repair or partial meniscectomy, while tears of the medial meniscus should be repaired
What are the indications for the different treatment options for longitudinal traumatic meniscus tears in stable knees?
Studies suggest that preservation of the meniscus in longitudinal tears is preferable to partial meniscectomy, and repair is recommended for medial meniscus tears, unstable tears, such as bucket handle and double longitudinal tears, and isolated meniscus tears.
What are the indications for the different treatment options for radial traumatic meniscus tears (except root tears) in stable knees?
The panel recommends that radial tears of zones 1 and 2 should be repaired to restore the integrity of the rim in patients with or without concomitant ACL reconstruction, but radial tears of zone 3 can be treated with a partial meniscectomy.
Should posterolateral meniscus root tears be repaired?
The panel notes repair of a posterolateral root tear decreases meniscus extrusion (in the sagittal plane) and the risk of osteoarthritis, and they recommend that such tears should be repaired.
Should a posteromedial meniscus root tear be repaired?
The panel also recommends repair of posteromedial tears to protect against consequent osteoarthritis, although they note that such tears are often degenerative rather than traumatic, and pre-existing osteoarthritis is likely to affect the outcome.
What is the optimal timing of a successful repair of stable and unstable meniscus tears?
The panel feels that acutely repaired meniscus tears achieve superior results compared to chronically repaired tears, but repair of a chronic tear may also achieve good to excellent results and repair should be attempted.
What is the best method to treat an acute, nonreducible (= locked) bucket handle meniscus tear in combination with an ACL tear in the office or emergency room?
The issue here revolves around the risk of arthrofibrosis which can be triggered if the knee is in an inflamed state at the time of surgery. If the ACL (anterior cruciate ligament) tear occurred several weeks or more before the locking incident, the panel recommends prompt repair of the meniscus and simultaneous reconstruction of the ACL. If the meniscus and the ligament were damaged at the same time but it is still within 60 hours of the injury, acute surgery may be delayed initially for a short while to allow any acute inflammation to calm down to avoid arthrofibrosis being triggered. If 60 hours has already passed, but there is still inflammation in the knee then the surgical options become more complicated. A one-stage procedure on both meniscus and ACL may protect the meniscus but lead ultimately to a stiff knee, while a two-stage procedure where the meniscus is repaired acutely but the ACL surgery delayed avoids this risk, but adds another of re-tearing the meniscus. The risk of meniscus re-tear increases by 1% with each 1-month interval from injury to surgery, so the ACL reconstruction should not be delayed too long, but the panel felt that the literature did not resolve exactly what the best time is to wait.
What are the indications for partial meniscus substitution?
There are apparently very few studies but the panel considers that the implantation of a partial meniscus substitution within the first surgery for partial meniscectomy should not generally be recommended, but it may be considered for patients with symptomatic failed meniscus surgeries.
Are biological techniques useful to enhance meniscus healing?
The discussion here included rasping and needling of the tear and opening up the medullary cavity, as well as the use of fibrin glue, fibrin clot, platelet-rich plasma and the local application of cells to the torn area. The panel were not able to specifically recommend any of these techniques because of a lack of relevant published studies.
